What is Root Canal Treatment?
Want to know more about root canal treatment? Watch our introductory video with Dr John McNamara
In addition to the information in the video, you'll find answers to the most common questions about root canal treatment below. If you have further questions, you are welcome to contact us by phone or email.
CLICK ON THE QUESTIONS BELOW TO READ OUR DETAILED ANSWERS
-
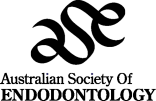
A guide to root canals
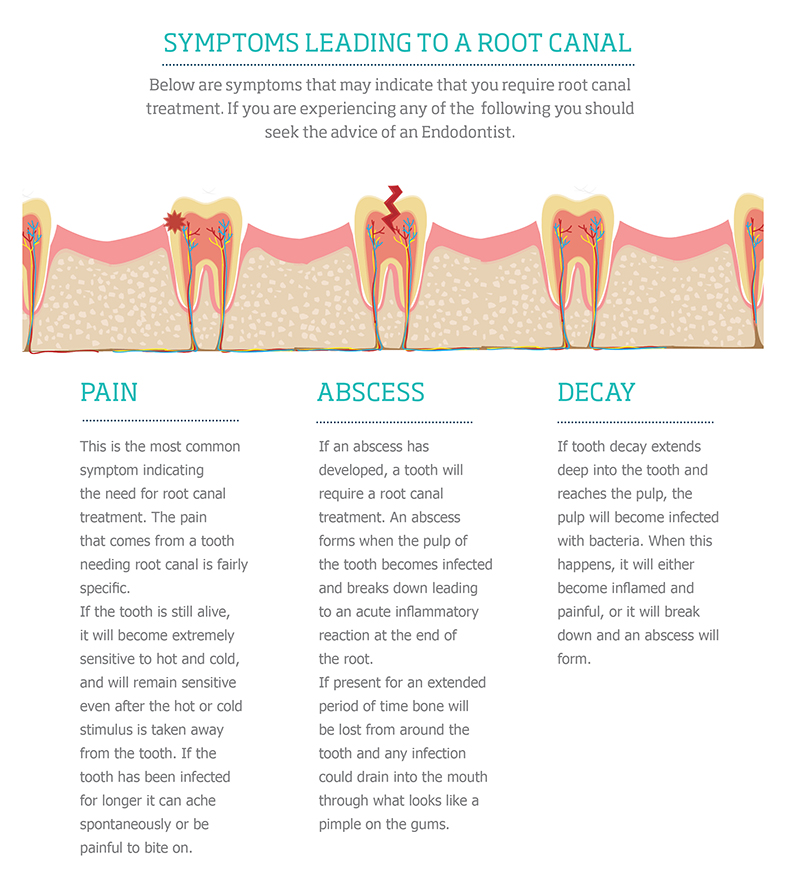
This infographic will give you an overview of root canals and root canal treatment, with further detail in our other FAQs. If you have any additional queries, you are always welcome to contact us.
-
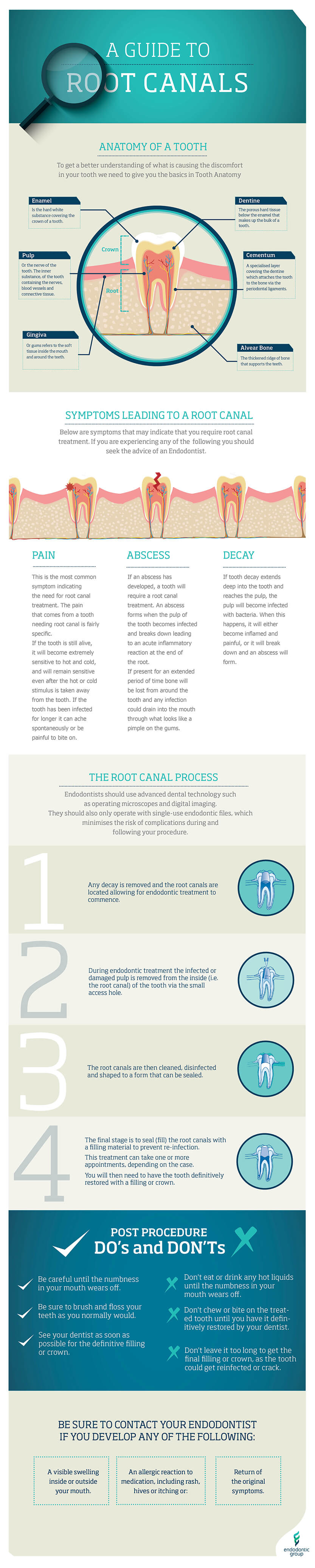
What’s the difference between a dentist and an endodontist?
Endodontists are dentists with additional postgraduate university training in root canal treatment, apicectomies, microsurgery, dental emergency and trauma management. They are not general dentists with an interest in root canal treatment. Endodontists are registered specialists with the Dental Board of Australia and it requires a minimum of three years additional postgraduate study to become an endodontist. You can verify that your dentist is registered in the speciality of endodontics here.
At the Endodontic Group we partner with general dentists to achieve and maintain optimal oral health for patients. A general dentist may refer a patient if they believe a better outcome would be achieved for your tooth having an endodontist perform your treatment. This is often the case for difficult or complex cases, teeth with additional roots, narrow or blocked canals, unusual anatomy, trauma or surgical procedures. Endodontists are better equipped for these situations because they encounter and treat these types of problems every day. Endodontists also have advanced technology available; routinely use microscopes and cutting edge equipment to perform specialist services.
General dentists are highly skilled in many areas, so here’s an overview of the difference between a dentist and an endodontist.
Endodontist Dentist Five years dentistry training at University 

Minimum of three years of postgraduate university training in Endodontics 
Registered specialist with the Dental Board of Australia 
Specialises in the diagnosis and treatment of the dental pulp, aetiology, prevention and treatment of diseases and injuries to the pulp and associated periradicular tissues 
Undertakes continuing education in new technology and procedures as an endodontist 
Routinely performs all treatment under a microscope, using cutting -edge technology and single use instruments 
Removes foreign objects (e.g. broken instruments) from canals using specialist equipment and technology 
Achieve more predictable outcomes for root canal treatment, root canal retreatment, apicectomies, dental emergency and trauma management 
Offers general and restorative dentistry including examinations, hygiene, fillings and crowns 
Extracts teeth 
Offers cosmetic dentistry such as veneers and tooth whitening 
-
Why can't my regular dentist do my root canal treatment?
While some general dentists will perform root canal treatment, they will often choose to refer you to a specialist to achieve the best possible outcome for your tooth. This is particularly the case in more complex cases, such as narrow or additional canals. Our endodontists are registered specialists with at least 3 years of additional specialist training beyond their undergraduate dental training. We only practise endodontics and use advanced equipment, so we have the experience and expertise to recognise the subtle differences in all the teeth we treat and ensure more predictable outcomes.
-
Why did my dentist refer me to an endodontist?
There are a multitude of reasons why your dentist may have referred you to see an endodontist. They may simply feel a better outcome can be achieved for your tooth by having an experienced, registered endodontic specialist perform the treatment. For instance, intricate or complicated cases often require specialist attention or equipment – this is often the case when there are additional roots, narrow or blocked canals, or unusual anatomy. Our endodontists encounter and treat these types of problems on a daily basis and are equipped to carry out treatment, particularly in emergencies, in a predictable and efficient matter.
-
Can my endodontist be my regular dentist too?
Our endodontists are registered specialists solely focused on root canal treatment and apicectomy or microsurgery. As such, we unfortunately cannot accommodate routine dental visits for our patients, but we do partner with your regular dentist to ensure the best possible outcome for your tooth. Exclusively providing endodontic treatment means that we can perform our best at carrying out root canal treatment while maintaining scheduling space for emergency patients who may be in pain.
-
Why has my health fund recommended a general dentist do my root canal?
Your health fund may refer you to a dentist on their preferred provider network or a dentist employed in one of their own clinics, which may be cheaper than being treated by your regular dentist or seeing a specialist for endodontic treatment. The health fund’s preferred provider may have a special interest in endodontics, but may not be a registered endodontist or root canal specialist. This Australian Dental Association article explains the health funds’ ‘preferred provider’ system in more detail.
Before seeking treatment with your health fund’s preferred provider, we suggest you consult with your regular dentist first and consider a consultation with a registered specialist so you have all your options in front of you. As registered specialists, our endodontists are always happy to work in partnership with your regular dentist to ensure the best possible outcome for you and your tooth.
-
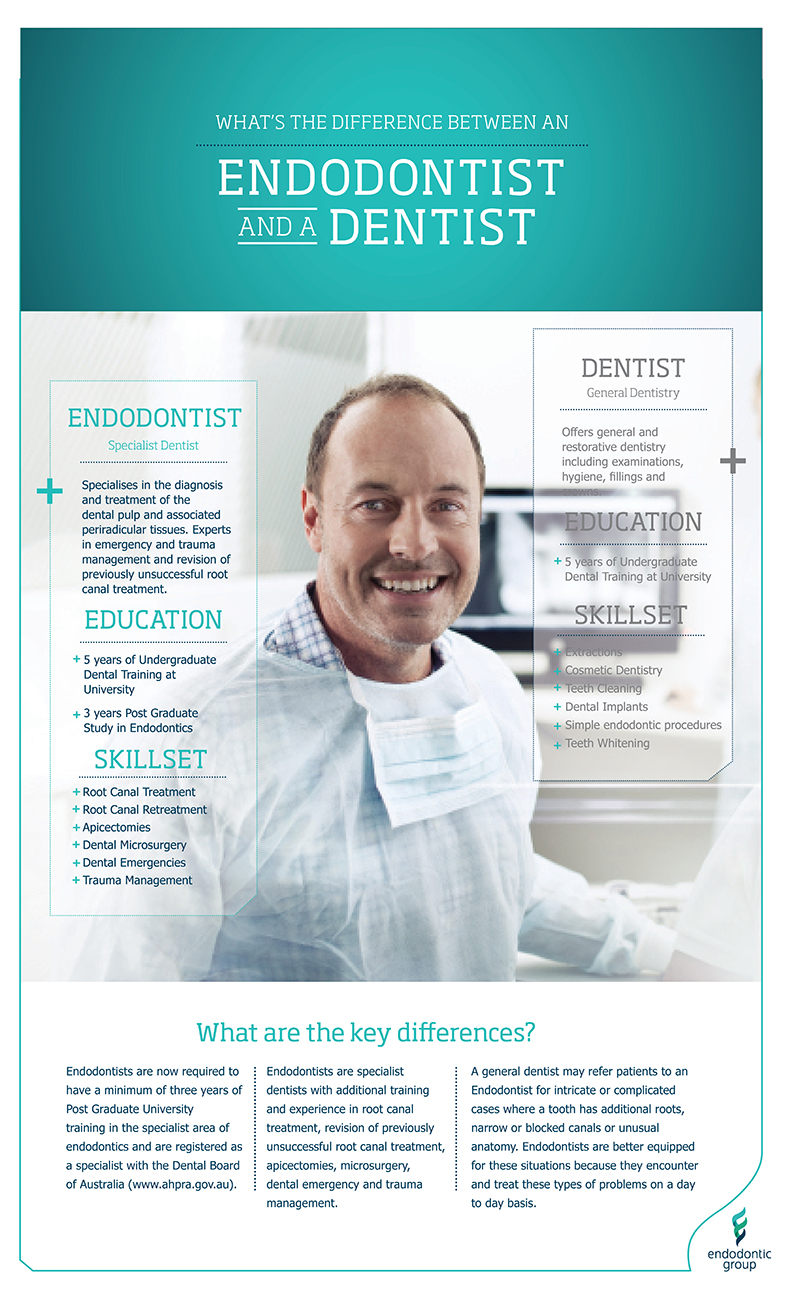
What is root canal treatment or root canal therapy?
Endodontics, pronounced en-do-don-tics, is a specialty area of dentistry that focuses on treatment inside the tooth. This includes treatment of the diseased dental pulp (or the nerve of the tooth), tooth root and surrounding tissues. Endodontic procedures are commonly referred to as root canal treatment or root canal therapy. Other specialist endodontic treatment includes root canal retreatment, apicectomies (a microsurgical procedure to remove a cyst or inflammatory tissue at the end of a tooth root) and management of dental emergencies. Endodontic treatment also includes management following dental trauma. When teeth are bumped, cracked or knocked out (avulsed), root canal treatment may be needed to save the tooth.
Root canal treatment commonly involves removing the inflamed or infected dental pulp. The dental pulp is the part of the tooth that allows us to feel temperature and alerts you to the presence of a problem like tooth decay. When bacteria enter the pulp through cracks, decay or following a bump or knock to the tooth, the pulp becomes inflamed and the tooth and surrounding area will become sore. Common symptoms are increased sensitivity to temperature (hot and cold), spontaneous aching, pain with biting or pressure and swelling. Any of those symptoms may indicate the need for root canal treatment.
The basic procedure can be seen in the diagram below. You might also like to visit our Video Gallery for more information.
-
What are the signs/symptoms that you may require treatment?
Some signs to indicate you may need endodontic treatment include:
- Continuous pain
- Extreme or prolonged sensitivity to hot or cold
- Discomfort when chewing
- Discolouration of a tooth
- Facial swelling
Sometimes you may have no symptoms at all, which is why regular check-up appointments with your dentist are so important.
-
How can endodontic treatment save your tooth?
By removing the infected pulp, cleaning and shaping the root canals, the endodontist relieves inflammation and pain. The root canals can then be filled and sealed. Afterwards, you return to your dentist, who places a crown or other restoration over the remaining tooth to protect it. Once restored, the tooth continues to function like any other tooth.

-
What is dental pulp? How does it become diseased?
The dental pulp is the name given to the soft tissue inside the canal or channel that runs through the root of your tooth. The dental pulp consists mainly of blood vessels, tissue fibres and some nerve fibres. The main function of the dental pulp is to regulate the growth and development of the tooth during childhood. Once the tooth is fully formed, nutrition for the tooth comes from the tissues surrounding the root, which means a tooth can function without its pulp and, in the majority of cases, can be kept permanently. After endodontic treatment the tooth is pulpless, so will no longer feel hot or cold. However, it is not a dead tooth - you will still experience the sensation of pressure when you chew on the tooth.
The most common cause of pulp damage is deep tooth decay, which allows bacteria to reach the pulp. The pulp may then become inflamed or infected. Products of infection may then spread through the opening at the tip of the root into the surrounding bone – an abscess could result and this may cause pain and swelling (Diagram A). Other causes of pulp damage include: traumatic blows to teeth, leakage around old or loose fillings, excessive wear of teeth, and cracked teeth. These processes can also lead to the infection of the pulp (Diagram B).


-
Implants or root canal treatment – which is best? Is the tooth worth saving or should I get it extracted?
In recent years, a misconception has developed amongst some dentists that implants have a ‘more predictable’ long-term outcome than root-filled teeth. In reality, when carried out to a high technical standard, root canal treatment is very successful. Statistically over 90% of root treated teeth will be present in ten years, which is comparable or better than most alternatives.
There are important factors to consider when deciding between root canal treatment and implants, and this decision should be made with the benefit of specialist advice. As we age, our overall medical health can often deteriorate and many conditions such as osteoporosis and diabetes will have an adverse impact on the long-term success of an implant. Similarly if you have periodontal disease or are a smoker, implants are generally more at risk of failing than a root filled tooth. Implants are also more likely to suffer from problems with gingival aesthetics (the appearance of the gums). Implants do not retain bone as well as a root-filled tooth and in the front of the mouth that can cause problems over time.
From an economic and practical perspective, root canal treatment and subsequent restoration of a tooth is in most cases cheaper and can be completed in a shorter period of time. In addition to saving money, root canal treatment avoids the need for patients to go without a tooth, or needing to wear a denture for any period of time.
The evidence is clear that good quality root canal treatment, combined with a good quality restoration leads to excellent long-term outcomes. For that reason, root canal treatment, retreatment or endodontic microsurgery should always remain the first treatment choice for patients with a restorable tooth experiencing pulpal disease.
-
Will root canal treatment work?
Your tooth will only be treated if there is a good chance it will last a long time. However, people have varied healing responses and some infections may respond differently, so no guarantees can be given. Studies have shown the majority of endodontic treatments are successful and uneventful. And we will inform you if your case is considered less favourable. Healing of the jawbone around the tooth can be slow and it’s important to have your tooth reviewed regularly to assess success. In rare cases, additional endodontic procedures may be required to aid the healing of the tissues around the tooth. Your endodontist will discuss this procedure with you if it becomes necessary.
-
How long will my root canal last? Will it need to be re-done?
When carried out to a high technical standard, endodontic (root canal) treatment is very successful. Statistically, over 90% of root treated teeth will be present in ten years, which is comparable (or better) than most alternatives. However, not all treatments are successful initially and some teeth can become reinfected at a later date.
There is a common misconception that teeth with ‘failed’ root canal treatment have a high risk of repeated failure and so they are often extracted instead of being retreated. The most common reason for unsuccessful initial treatment is generally persistent bacteria in the tooth. This usually occurs because of inadequate cleaning of the root canals. It’s common during retreatments for endodontists to be able to clean closer to the root tip, locate and clean extra canals and access complicated parts of the inside of the root such as fins, isthmuses and lateral canals. These extra canals and complex hidden anatomical features are generally only visible with a microscope and able to be accessed with specialised tools and techniques.
Reinfection that occurs several years after the initial treatment generally occurs because of more bacteria entering the tooth. This is commonly due to leaking fillings, decay or cracks that have developed in the tooth. Using a microscope, endodontists are able to diagnose these problems quickly to ensure the infection is removed so the problem does not reoccur after retreatment.
Historically it was thought that endodontic retreatment carried a lower success rate than initial treatment. However, with newer techniques and equipment like microscopes and rotary endodontic files, it’s now possible for endodontists to achieve the same high success rate as initial treatment.
-
Is there an alternative to endodontic treatment?
Endodontic treatment is a safe procedure and it’s undertaken to save your tooth. There is no real substitute for your own tooth – it’s far more efficient in chewing and biting than an artificial tooth. The only alternative method of removing the infection is to extract your tooth. If you do not have the tooth replaced with an artificial one, the adjoining or opposing teeth may shift, interfering with biting and chewing. Loss of a tooth may also lead to other complex problems including decay of other teeth, jaw joint and jaw muscle problems, and gum disease. Replacing your tooth with an artificial tooth often involves more complex treatment such as bridgework or implants, which is more costly and time consuming.